OVERDOSE! Know how to SAVE A LIFE!
What is Narcan (Naloxone)?
Narcan is the brand name for naloxone hydrochloride, a medication that acts as an opioid antagonist. It works by binding to opioid receptors in the brain, displacing opioids like heroin, fentanyl, or prescription painkillers, and rapidly reversing the life-threatening effects of an overdose, such as slowed or stopped breathing.
Naloxone is safe to administer even if you’re unsure if an opioid overdose is occurring, as it has no effect on someone not exposed to opioids. It’s available over-the-counter in many places and is commonly used by first responders.
Other forms of naloxone exist beyond the Narcan brand, including generic versions.Key signs of an opioid overdose include:
- Slow, shallow, or stopped breathing
- Unresponsiveness (no reaction to shouting or sternum rub)
- Blue or gray lips/fingernails
- Pinpoint pupils
- Gurgling or snoring sounds
In any suspected overdose, always call 911 immediately (or have someone else call) before or right after administering naloxone, as its effects are temporary (30-90 minutes) and the person may need further medical care.
Perform rescue breathing or CPR if trained and if the person isn’t breathing.Below are step-by-step instructions for administering naloxone in the requested forms: nasal spray (e.g., Narcan), sublingual (not standard, explained below), and injection. These are based on standard guidelines; consult local health authorities or product instructions for specifics.
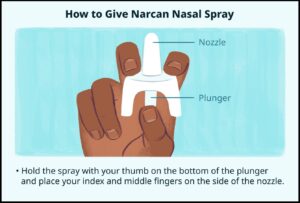
Nasal Spray Administration (e.g., Narcan or Generic Naloxone Nasal Spray)
This is the most common and user-friendly form for laypeople, available as a prefilled, single-dose device (typically 4 mg per spray).
- Lay the person on their back and support their neck to tilt the head back slightly.
- Check for responsiveness and breathing; if none, call 911.
- Remove the nasal spray from its packaging—do not test or prime it.
- Hold the device with your thumb on the bottom of the plunger and your first two fingers on either side of the nozzle.
- Gently insert the nozzle tip into one nostril until your fingers touch the bottom of the nose.
- Press the plunger firmly to deliver the full dose.
- Remove the device and monitor the person. If no response (e.g., no breathing restoration) after 2-3 minutes, administer a second dose in the other nostril using a new spray.
- If breathing doesn’t return, start rescue breathing: Tilt head back, pinch nose, and give one breath every 5 seconds.
- Place the person in the recovery position (on their side) once they respond, and stay with them until help arrives.


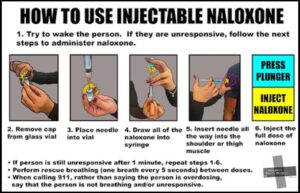
Injection Administration (Intramuscular, Subcutaneous, or Intravenous Naloxone)Injectable naloxone comes in vials (requiring a syringe) or prefilled syringes/auto-injectors (e.g., 0.4 mg to 2 mg doses).
It’s typically administered intramuscularly (IM) into a muscle for laypeople, subcutaneously (SC) under the skin, or intravenously (IV) by medical professionals.
Doses vary; start with 0.4-2 mg for adults.
- Lay the person on their back and check for responsiveness/breathing; call 911 if not already done.
- If using a vial: Draw the dose (e.g., 0.4-2 mg) into a syringe with a needle (21-25 gauge, 1-1.5 inches for IM).
- Choose the injection site: For IM, outer thigh, upper arm, or buttocks; for SC, abdomen or thigh; for IV, a vein (requires training—avoid if untrained).
- Clean the site with alcohol if possible.
- Insert the needle at a 90-degree angle for IM/SC and inject the dose steadily.
- Remove the needle and apply pressure if bleeding.
- Monitor for response. If no improvement after 2-3 minutes, give another dose (up to 10 mg total may be needed in severe cases, especially with potent opioids like fentanyl).
pmc.ncbi.nlm.nih.gov
- Perform rescue breathing if needed, as described above.
- Place in recovery position once responsive.
For auto-injectors (e.g., Evzio): Follow device instructions—press against outer thigh until it clicks, hold for 5 seconds.


Sublingual Administration
Sublingual (under the tongue) administration of pure naloxone is not a standard or FDA-approved method for opioid overdose reversal, as naloxone has poor sublingual bioavailability (around 4-25% depending on formulation) and is not formulated for this route in emergency settings.
Standard naloxone products are not available in sublingual form for overdose treatment.However, in rare reported cases, sublingual buprenorphine/naloxone (e.g., Suboxone tablets or films, which combine buprenorphine for opioid dependence treatment with naloxone to deter misuse) has been used off-label to reverse heroin or other opioid overdoses when no other options were available.
This is not recommended as a first-line approach, as it can precipitate withdrawal symptoms and is less reliable than dedicated naloxone.
If considering this in an emergency (only if pure naloxone is unavailable):
- Confirm overdose signs and call 911.
- Place a Suboxone tablet or film (e.g., 8 mg buprenorphine/2 mg naloxone) under the person’s tongue; allow it to dissolve (do not chew or swallow).
- Monitor closely; effects may take longer than with nasal or injection (up to 15-30 minutes).
- Provide rescue breathing if needed.
- Administer additional doses or switch to standard naloxone if possible; seek immediate medical help.
This method carries risks like incomplete reversal or withdrawal, so prioritize approved forms. For opioid dependence treatment (not acute overdose), sublingual buprenorphine/naloxone is commonly prescribed.
Additional Notes
- After reversal, the person may experience withdrawal symptoms like nausea, agitation, or pain—reassure them and prevent further opioid use to avoid re-overdose.
- Naloxone doesn’t treat non-opioid overdoses; if unsure, administer anyway and get help.
- Store naloxone at room temperature; check expiration dates.
- For training or access, contact resources like SAMHSA’s helpline (1-800-662-HELP).
samhsa.gov